When members see a health care provider, they often receive bills and receipts that only include part of the information we need to process a reimbursement. For the full context, we need an itemized bill or statement.
To make sure you know what you’re looking for, and that the provider has sent you the document you need, here’s an outline of what should be included on an itemized bill and why we need it.
What Is An Itemized Bill?
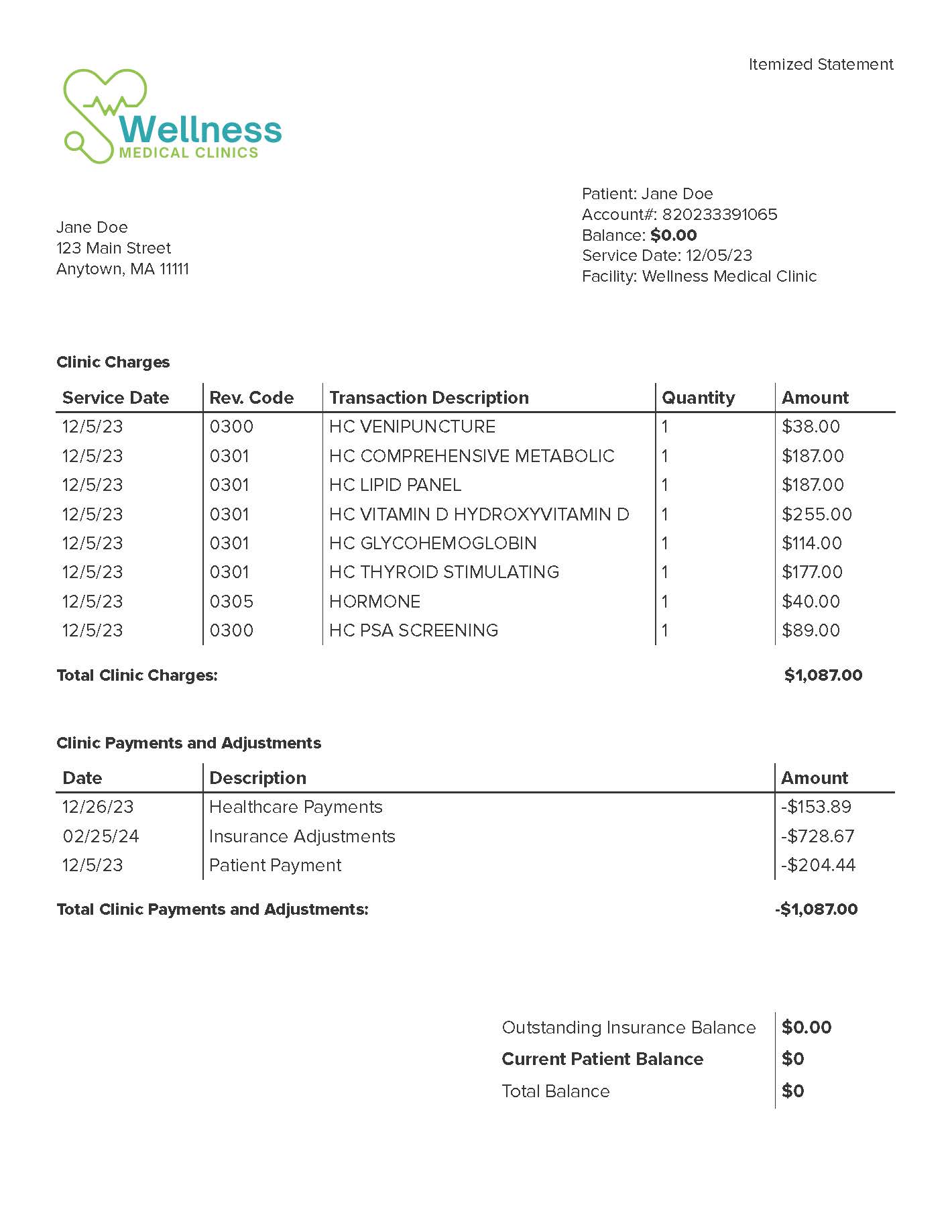
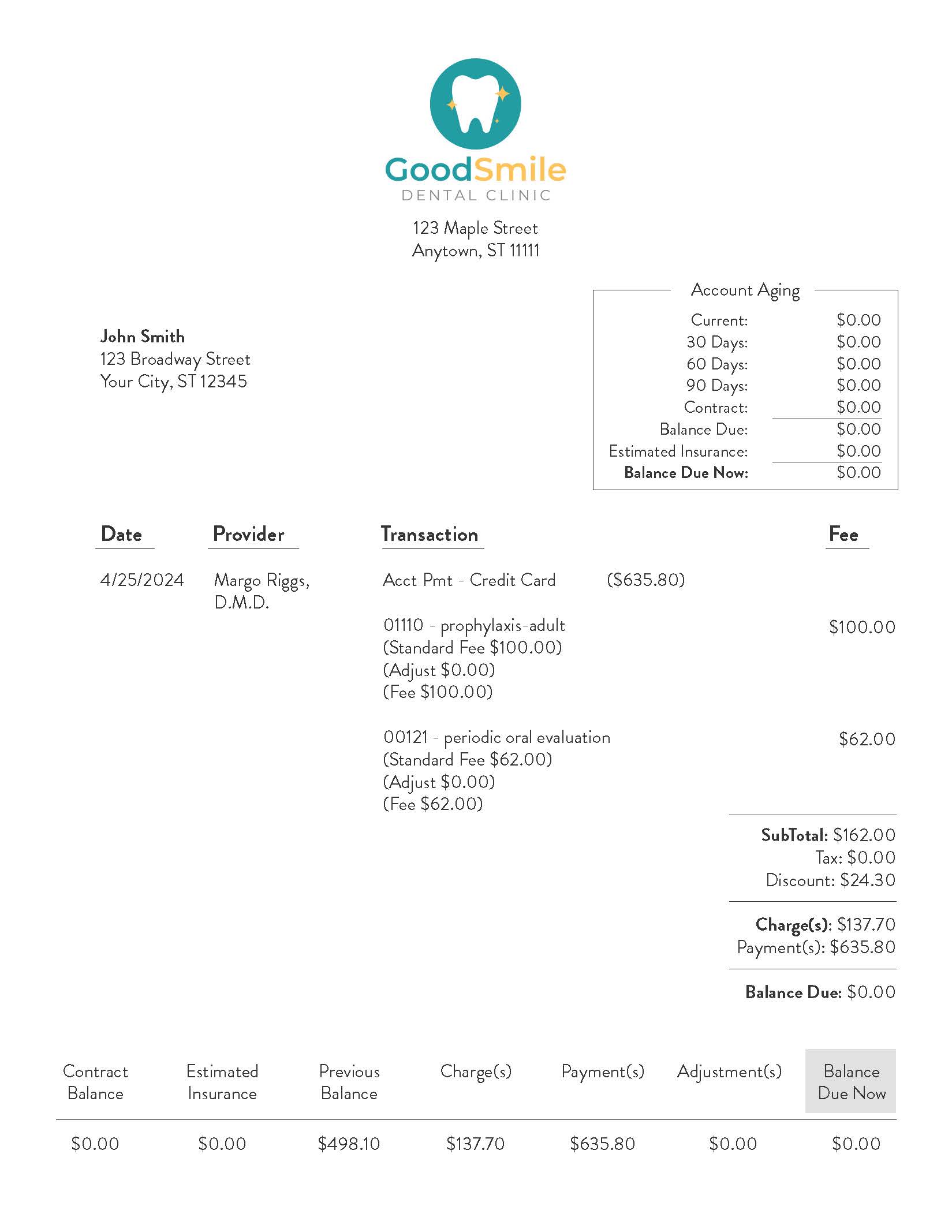
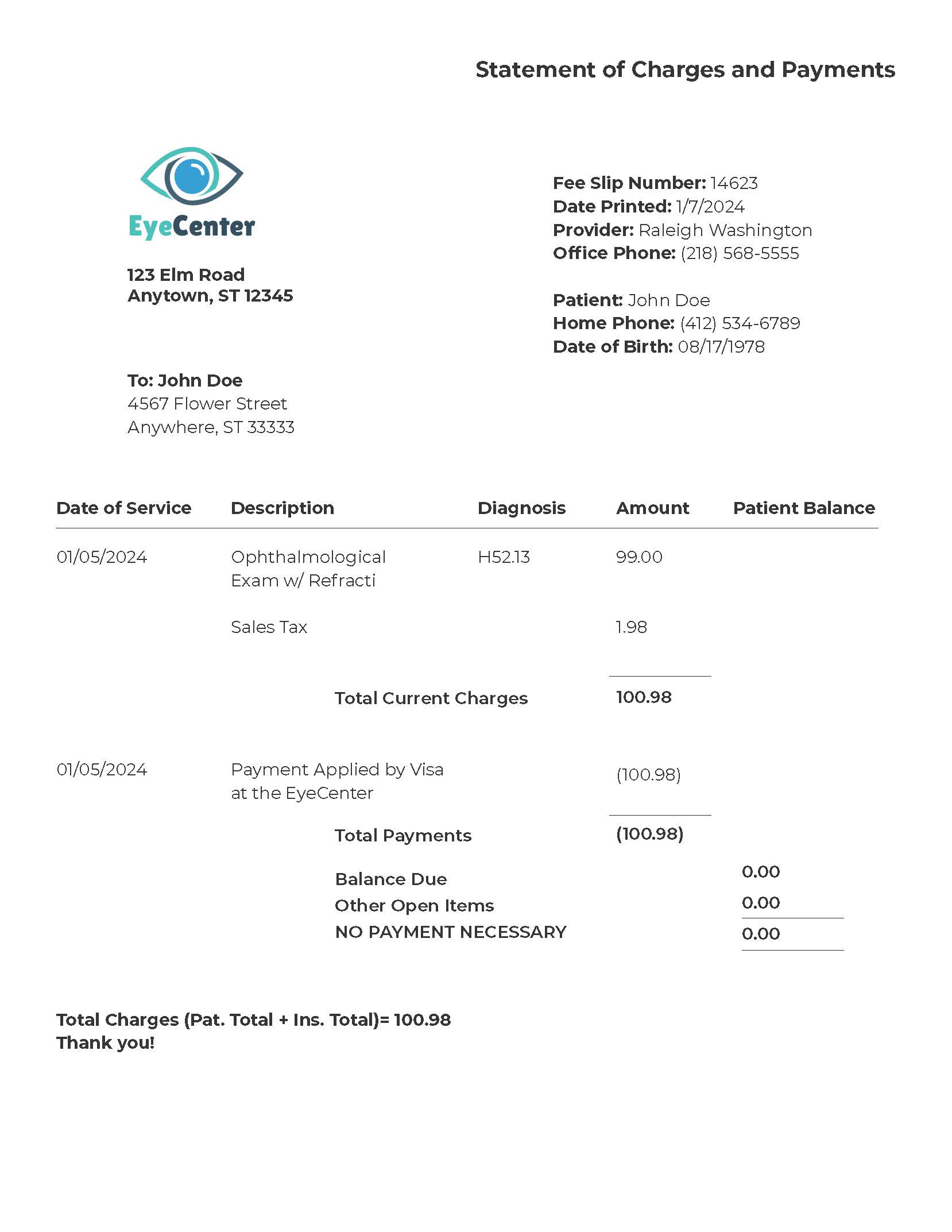
An itemized bill or statement will include:
- Provider’s name and contact information (or the fitness provider’s name in the case of a gym membership)
- Patient’s name
- Date of service
- Breakdown and description of each service performed, including a service code
- Charge amount for each service
- Final patient responsibility after any provider discounts or insurance payments (if applicable)
Here are a few examples of itemized bills that include each piece of the necessary information:
What Is Not An Itemized Bill?
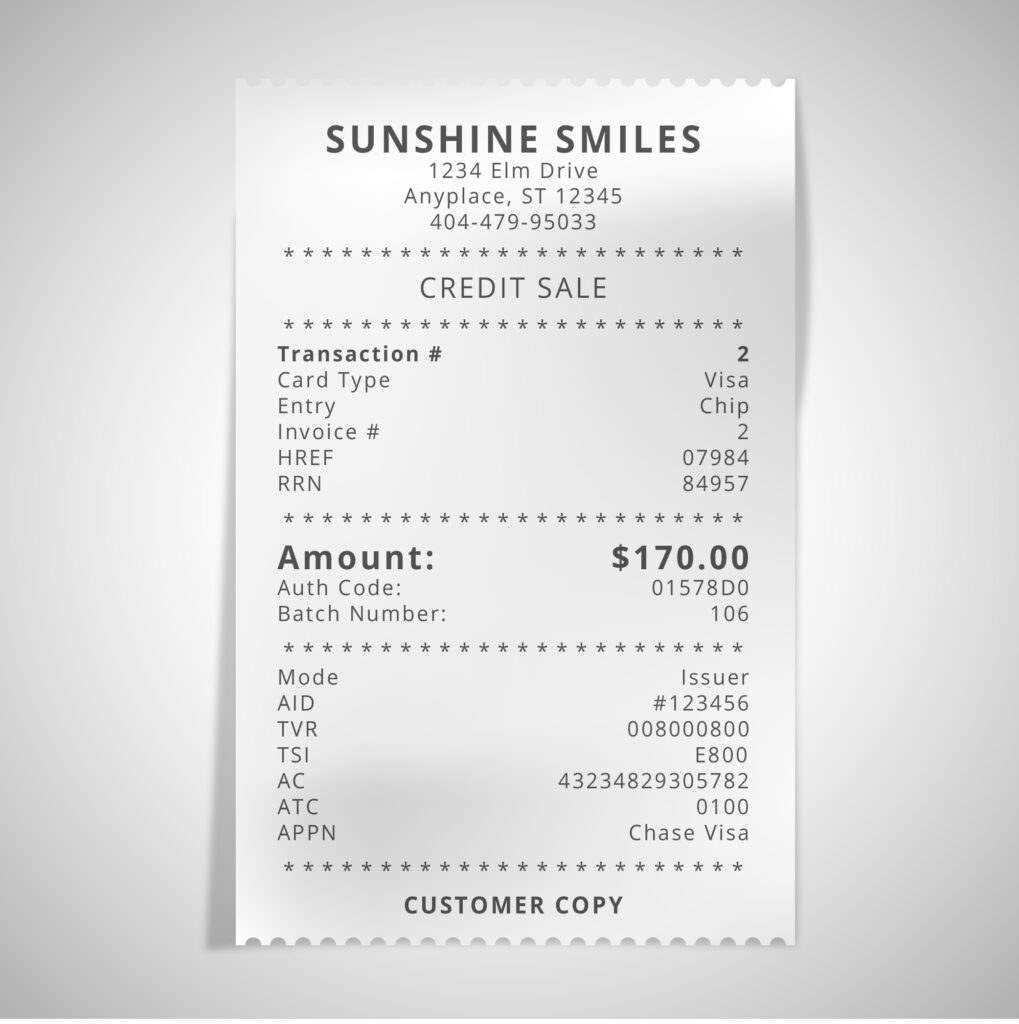
A credit or debit card receipt.
If you are required to pay at the time of service, you will often receive a non-itemized receipt that does not include the services performed and may not even list the patient’s name. In order to confirm that the gym membership or medical service billed is for a member and that it is for an eligible expense, we need to see that information.
Here is an example of a non-itemized receipt:
A non-itemized bill, invoice, or receipt.
You may also receive a request for payment or a receipt that looks more official and which may include your name, the provider’s contact information, the date of service, and the amount charged. Because these have some of the information we need, it’s understandable that many members often think these documents are sufficient to process a reimbursement.
However, as you can see from the example below, these bills do not include specific services performed or the charges for each service.
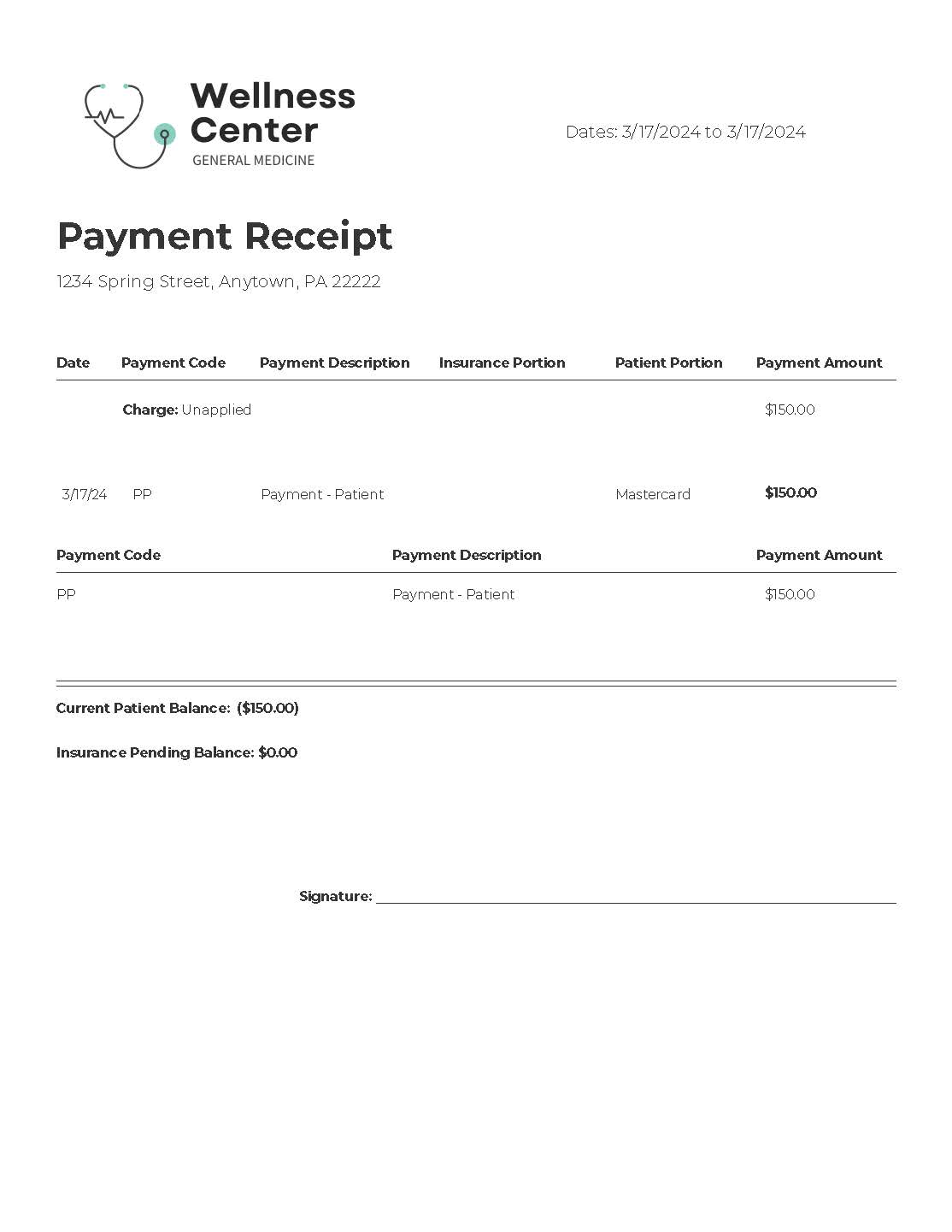
If you note that the document you receive from your provider looks like this example and does not include service-specific codes, descriptions, and charges, then you will have to request an itemized statement or bill.
Why Do We Need An Itemized Bill?
When we have an itemized bill or statement, we can check the specific services rendered against our list of eligible services. This makes our reimbursements to you a lot faster. After receiving an itemized bill, we can process a reimbursement within a few business days.
How Do You Request An Itemized Bill?
If you have received a non-itemized receipt or bill from your provider, you can typically call, request the billing department, and explain that you need to receive an itemized bill either by email or by mail.
Most providers will not ask you why but if they do you can explain that you have an employee assistance program (EAP), that is not insurance and may reimburse your eligible expenses.
Once you receive the itemized document and compare it against the examples and information above to ensure that it has the needed information, you can submit it to us through this form for a rapid review and reimbursement of eligible expenses.
If you have questions about itemized bills, eligible expenses, or your membership, don’t hesitate to contact us at any time at members@healthaccesssolutions.com or (800) 606-1135.
